
The field of virtual healthcare is rapidly expanding. It serves an increasingly important role in the diagnosis and treatment of illness and in assisting consumers in maintaining and improving their well-being. The globe has finally gotten some much-needed aid from virtual hospital solutions.
Keep reading for more information, including its benefits and drawbacks.
1. What is Virtual Healthcare?
The term “virtual health” refers to a set of services that healthcare providers can use to enhance the quality of treatment. Which they deliver to patients via the use of various digital technologies. Additionally, it facilitates communication between doctors and their patients, irrespective of their geographical location. Instead of traveling to a doctor’s office, patients have the option to video chat with a doctor or expert.
2. Benefits of Virtual Healthcare
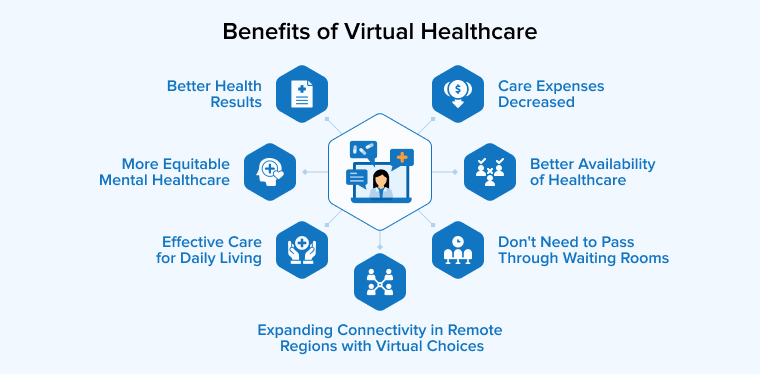
In the face of both extraordinary and mundane challenges, virtual care provides answers that guarantee continuity of care. These are only a few of the many long-term advantages.
2.1 Effective Care for Daily Living
The effectiveness of virtual care is a great advantage. Particularly if you have fast visits for managing chronic illnesses, checking in, or anything else.
Everything from unusual situations and demanding routines to fears of the COVID-19 epidemic and the reality of everyday life may be accommodated with virtual care.
Instead of calling to schedule an appointment, you may just send a message to your physician with any questions or concerns you may have using the messaging tools of your telehealth platform.
2.2 Better Availability of Healthcare
Patients now have more ways than ever to communicate with their primary care physicians, health coaches, mental health specialists, nurse practitioners, and physical therapists through virtual care. Which is a great alternative to in-center consultations.
It’s another way for workers to get the treatment they need whenever they need it, regardless of when they work.
2.3 Better Health Results
When combined with a health outcomes-based care paradigm, virtual care expands the comprehensive, in-person experience of in-center visits. Patients can take a more active role in achieving their health objectives, and clinicians can better understand their conditions. Because of the trusted connections that develop through virtual care.
2.4 Care Expenses Decreased
Virtual care streamlines the healthcare system by reducing demand for additional facilities and boosting the use of primary care services, such as preventative and regular dental treatment. Emergency room visits, hospital stays, specialist care, and urgent care fall under this category.
2.5 More Equitable Mental Healthcare
There have been more barriers to behavioral healthcare for rural patients in the past, but this is no longer an issue with virtual treatment. At a time when over 40% of American people report having mental health issues, virtual care sessions are frequently the primary cause of these visits.
2.6 Expanding Connectivity in Remote Regions with Virtual Choices
Traditional healthcare access is declining in rural regions, which is contributing to the rise of virtual care services. Even though less than 8% of the nation’s medical professionals work in rural locations, over 20% of Americans call these places home. Virtual choices allow patients to contact specialists through any internet-connected device, even if they can’t get the service they need locally. Because of this, people and their families don’t have to drive far to get the medical treatment they need and fill their prescriptions.
2.7 Don’t Need to Pass Through Waiting Rooms
Have you ever had an appointment at an urgent care center or elsewhere, only to be stuck in a freezing waiting area for hours? Waiting in a virtual room is more tolerable, particularly if you’re waiting at home in bed or while having lunch.
3. Drawbacks of Virtual Healthcare
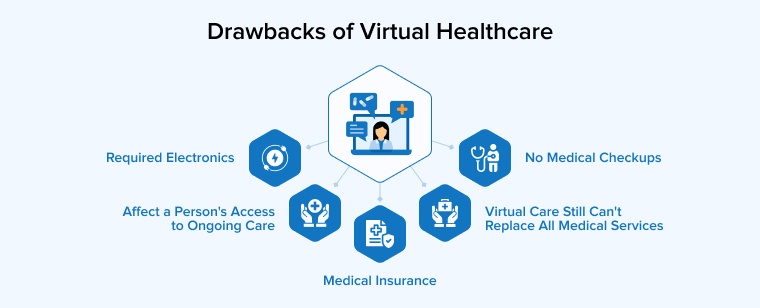
Let’s discuss some disadvantages of Virtual Healthcare.
3.1 No Medical Checkups
What may be accomplished through telehealth is not without its restrictions. For instance, it is not feasible to do physical examinations using a computer screen. The usefulness of telehealth diminishes when compared to the ease and accuracy of a physical examination or imaging test.
3.2 Required Electronics
A computer, smartphone, or other internet-connected device is usually required to carry out a virtual care visit. Although some virtual care visits may be conducted via messaging apps or phones, dependable technology is still required. Telehealth often lacks even the most basic instruments needed to take vital signs during in-person appointments, including thermometers and blood pressure cuffs.
3.3 Medical Insurance
Telehealth visits are becoming more common, and although some insurance companies do pay them, the majority do not. You might not be able to use your insurance with some virtual services. Think about and investigate this thoroughly before agreeing to a virtual care appointment; if you have particular issues about telehealth benefits or costs, call your insurance provider.
3.4 Affect a Person’s Access to Ongoing Care
Imagine for a moment if the healthcare professionals you normally connect with are different from the ones you interact with virtually. Then there’s a higher chance of incorrect diagnosis, medical mistakes, or improper treatment as they might not have access to your whole medical history. This information gap works in both directions: if your primary care physician doesn’t have access to your virtual visit notes, they may overlook crucial details about your health and fail to give you the treatment you need.
3.5 Virtual Care still can’t Replace All Medical Services
Patients must be present in person with a healthcare provider for some tests, medical treatments, and operations.
4. How Virtual Healthcare Differs from Telemedicine?
Telemedicine is the practice of providing medical care to patients using electronic means rather than face-to-face interaction. Remote patient assessment and detection can be accomplished using phone, video, or e-mail. One use of telemedicine is when a patient reports a high temperature but otherwise feels well enough to receive a prescription for over-the-counter cold medication after consulting with a doctor over the phone.
The phrase “virtual care” encompasses a lot more than just healthcare. All interactions between a healthcare provider and their patients are covered. An example of virtual care might be a nurse calling a patient to see how they are doing after the operation, or remotely tracking vital signs using wearables.
A lot of people get telehealth and virtual healthcare mixed. In reality, telehealth allows patients to communicate with their healthcare providers and vice versa; it is an element of the virtual healthcare system. When it comes to serving patients who are located in different locations, there are several options available. One such benefit of virtual healthcare is the ability for patients in underserved or otherwise inaccessible places to get better care through the use of real-time contact between a real healthcare professional and a patient.
By leveraging technology, virtual health enhances the delivery of healthcare. Researchers have shown that virtual health programs have several benefits for clinicians and patients alike, including financial savings, better clinical results, more patient participation, and wider access to treatment.
5. How does Virtual Healthcare Work?
While the term “virtual medical care” can apply to a variety of services, for a patient and physician to securely communicate by video chat, phone, message, or any other means, a platform that complies with HIPAA regulations is required. Even if you don’t have an appointment with your doctor, you might be able to get your blood tested by visiting a lab or using a mail-in kit. Virtual care can be accessible through your primary care physician’s office or by searching online for terms like “virtual health” and many more.
Starting with virtual health visits might seem different for everyone since different platforms have distinct approaches. No matter what you name it, telehealth (or virtual care) allows patients to consult with doctors without leaving the comfort of their own homes.
6. Conclusion
A significant portion of healthcare’s future will be devoted to virtual services. To stay ahead of the competition and capitalize on developing technology, healthcare systems, apps, and solutions, healthcare stakeholders will most likely have to implement new business models.
To stand in the healthcare industry, reach more people, provide better service, and overcome operational limitations, health systems must adopt virtual healthcare. Second views, consultations, managing chronic diseases, and online monitoring of specific ailments are all areas where virtual healthcare could prove helpful.
Healthcare systems need to move quickly to address the growing need for realistic solutions. That can keep up with the expanding capabilities and widespread usage of virtual healthcare.
FAQ
What is the difference between telehealth and virtual health?
Virtual health encompasses more than just telehealth; telehealth is just one component of virtual health. The word “telehealth” is commonly used to describe the use of technology to provide healthcare services. That were previously only available in person, such as online video consultations with doctors or nurses.
What is virtual care in healthcare?
In healthcare, “virtual care” usually refers to two distinct services: telemedicine and remote patient monitoring. In telemedicine, doctors and other medical professionals utilize videoconferencing technology to virtually examine, diagnose, and keep tabs on patients. Those who are at risk for developing a chronic illness or who are already living with a chronic ailment can use virtual care through remote patient monitoring.






Comments
Leave a message...